Table of contents:
Introduction
Pulmonary embolism (PE) is a significant and potentially life-threatening medical condition that occurs when a blood clot blocks one or more arteries in the lungs. The severity of PE stems from its ability to rapidly impair lung function and compromise oxygen circulation throughout the body. Timely diagnosis and intervention are crucial, as delays in treatment can lead to severe complications, including chronic health issues and in some cases, mortality.
Recent statistics highlight a concerning rise in the incidence of pulmonary embolism, shedding light on the pressing need for increased awareness and understanding of this condition. Despite advancements in medical research and treatment methods, many individuals remain unaware of the risks and symptoms associated with PE, often attributing their symptoms to less severe ailments. This lack of recognition underscores the importance of education and awareness in the early detection and prevention of pulmonary embolism.
Understanding pulmonary embolism is paramount not only for healthcare professionals but also for the general public. Recognizing the signs and symptoms, being aware of the risk factors, and knowing when to seek medical attention can significantly impact the prognosis. Preventative measures, when implemented early, can effectively reduce the risk of developing PE. By spreading knowledge and encouraging proactive health measures, we can mitigate the risks associated with pulmonary embolism, ultimately saving lives and improving health outcomes.
This blog post aims to provide comprehensive insights into the causes, symptoms, and prevention of pulmonary embolism, offering valuable information that can guide individuals in recognizing and addressing this critical health issue. By fostering a greater understanding of PE, we hope to enhance early detection and encourage steps toward prevention, ensuring better health and safety for all.
What is Pulmonary Embolism?
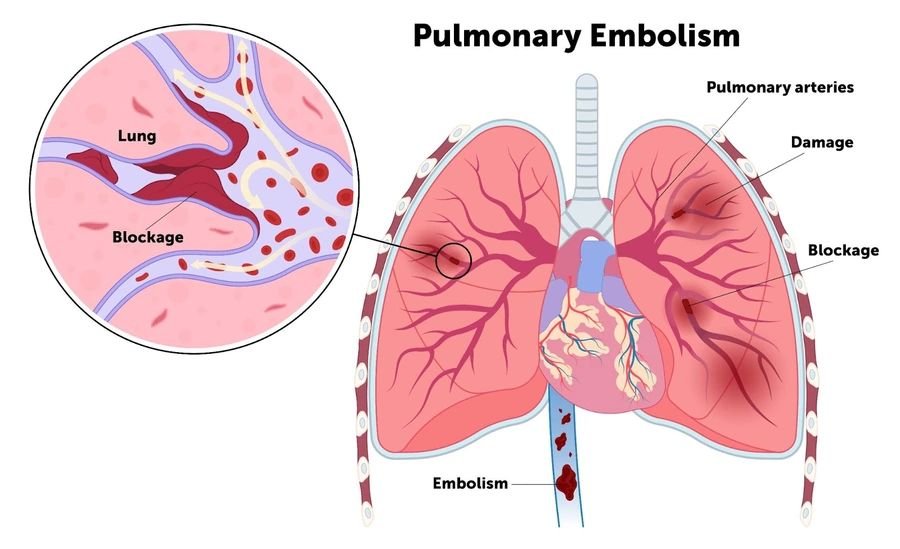
Pulmonary embolism (PE) is a serious medical condition that occurs when a blood clot, often originating from the deep veins of the legs, blocks one of the pulmonary arteries in the lungs. This process often starts with a condition known as deep vein thrombosis (DVT), where blood clots form in the deep veins, usually in the legs. These clots can travel through the bloodstream, move towards the heart, and eventually become lodged in the pulmonary arteries. The blockage created by the clot prevents blood from reaching the lungs properly.
The obstruction of the pulmonary arteries by a blood clot can have several severe consequences. One of the immediate effects is damage to lung tissue due to the restricted blood flow. The areas of the lung that are deprived of blood can begin to die, resulting in impaired lung function. As a consequence, the level of oxygen in the blood decreases, compromising the oxygen supply to various organs and tissues throughout the body.
This reduction in oxygen levels can profoundly impact the function of major organs, including the heart, brain, and kidneys. When the heart is forced to work harder to push blood through the blocked arteries, it can lead to strain and, in severe cases, heart failure. Similarly, inadequate oxygen supply to the brain may result in dizziness, fainting, or neurological symptoms. In the kidneys, reduced blood flow can impair their ability to filter waste products from the body.
Recognizing the symptoms and understanding the risk factors associated with pulmonary embolism is crucial for prompt diagnosis and effective treatment. Early intervention can significantly improve outcomes and reduce the long-term complications associated with this potentially life-threatening condition. Thus, knowledge and awareness about PE are essential for preventing its occurrence and ensuring timely medical attention.
Causes and Risk Factors
Pulmonary embolism (PE) predominantly occurs when a blood clot, often originating from the leg veins in a condition known as deep vein thrombosis (DVT), travels through the bloodstream and lodges within the pulmonary arteries. This blockage can critically impede blood flow to parts of the lung, leading to severe complications. Understanding the various causes and risk factors associated with PE is crucial for effective prevention and management.
One primary cause of pulmonary embolism is prolonged immobility. Extended periods of inactivity, such as those encountered during long flights or bed rest following surgery, increase the risk of clot formation. Moreover, recent surgeries, particularly those involving the hips or legs, can elevate this risk due to factors such as reduced movement and potential damage to blood vessels.
Certain medical conditions also contribute significantly to the likelihood of developing PE. For instance, some types of cancer, especially those affecting the pancreas, lungs, and ovaries, can induce hypercoagulability, a state where blood clots more readily. Genetic predispositions also play a role; individuals with inherited blood clotting disorders have a higher propensity to form clots, which can lead to pulmonary embolism.
Beyond these primary causes, several risk factors further heighten the likelihood of developing PE. Age is a critical factor, with individuals over 60 at a greater risk. Obesity compounds this risk due to increased intra-abdominal pressure and general immobility. Lifestyle choices like smoking can damage blood vessels and elevate clot risk, while pregnancy and the postpartum period similarly increase clotting potential due to hormonal changes and reduced mobility.
Additionally, the use of hormonal contraceptives or hormone replacement therapy can contribute to a greater clotting risk. Pre-existing heart diseases, especially those affecting heart rhythm and pumping efficiency, further complicate the circulatory system, creating a conducive environment for clot formation. Awareness of these varied causes and risk factors can aid in early identification and preventive strategies for pulmonary embolism.
Symptoms and Diagnosis
Pulmonary embolism (PE) is a serious condition characterized by the sudden blockage of one or more pulmonary arteries in the lungs. The symptoms of PE can vary significantly in intensity, but they typically include sudden onset of shortness of breath, which may occur at rest or during physical activity. Patients often experience chest pain that can become more severe with deep breaths, mimic the pain associated with a heart attack, and may radiate to the shoulder, arm, neck, or jaw.
Other common signs include a persistent cough, sometimes accompanied by bloody or blood-streaked sputum. Rapid or irregular heartbeats, known as palpitations, are also associated with pulmonary embolism. Some individuals may experience lightheadedness, dizziness, or even fainting episodes due to the decreased oxygen levels in the blood caused by the obstructed blood flow in the lungs.
The diagnostic process for pulmonary embolism is multifaceted and begins with a thorough clinical evaluation, including a detailed patient history and physical examination. One of the initial steps in diagnosing PE is the D-dimer blood test, which measures the presence of a substance that is released when blood clots dissolve. Elevated levels of D-dimer may suggest the need for further diagnostic procedures.
CT pulmonary angiography (CTPA) is a commonly employed imaging test that provides detailed pictures of blood vessels in the lungs, allowing direct visualization of any possible clots. In cases where CTPA is contraindicated or additional evaluation is required, a ventilation-perfusion (V/Q) scan might be performed. This scan assesses both airflow (ventilation) and blood flow (perfusion) in the lungs to detect abnormal regions.
Ultrasound of the legs, particularly a Doppler ultrasound, is often used to identify deep vein thrombosis (DVT), a common source of emboli that can travel to the lungs. In certain situations, magnetic resonance imaging (MRI) may also be utilized for its high level of detail and absence of radiation exposure, notwithstanding its less frequent use compared to other modalities.
Treatment Options
Pulmonary embolism (PE) requires prompt and effective treatment to prevent complications and improve recovery outcomes. The primary treatment modalities for pulmonary embolism can be broadly categorized into pharmacological therapies and surgical interventions.
Anticoagulant medications, such as heparin and warfarin, are commonly prescribed to individuals diagnosed with a pulmonary embolism. These drugs play a crucial role in preventing the formation of new blood clots and stopping the growth of existing ones. Heparin, administered intravenously or via subcutaneous injection, acts rapidly and is typically used in the acute setting. Meanwhile, warfarin, an oral anticoagulant, requires regular monitoring and dosage adjustments but is often used for long-term management to maintain therapeutic anticoagulation.
For severe cases where immediate clot resolution is necessary, thrombolytic therapy or ‘clot busters’ like alteplase may be employed. These potent medications help dissolve existing clots rapidly, thereby restoring normal blood flow. Thrombolytics are usually reserved for life-threatening circumstances due to their risk of causing significant bleeding.
In instances where medication alone is insufficient or unsuitable, surgical interventions might be necessary. Embolectomy, a surgical procedure that removes the clot directly from the pulmonary arteries, is one such option. While generally considered a last resort due to its invasive nature, advancements in surgical techniques have made it a viable option for certain patients.
Another less invasive technique is catheter-directed thrombolysis. This procedure involves the insertion of a catheter directly into the clot, allowing for the targeted delivery of thrombolytic drugs. This method enables more controlled clot dissolution and minimizes systemic exposure to potent medications.
Early and appropriate treatment of pulmonary embolism is imperative to reduce the risk of complications such as recurrent embolism or chronic thromboembolic pulmonary hypertension. Tailoring the treatment approach to individual patient needs can significantly improve prognosis and aid in a smoother recovery process.
Prevention and Lifestyle Tips
Mitigating the risk of pulmonary embolism (PE) involves adopting several proactive lifestyle habits and precautions. Incorporating regular physical activity into daily routines is crucial. Engaging in exercises such as walking, swimming, or cycling can enhance blood circulation and reduce the likelihood of blood clots forming. It is equally essential to stay hydrated; proper hydration aids in maintaining optimal blood viscosity and venous return.
Avoiding prolonged immobility is another vital preventive measure, especially during extended travel or post-operative recovery. During long flights or car rides, make it a point to stand, stretch, or walk at intervals. After undergoing surgery, follow physician-recommended protocols to encourage early mobilization. Many healthcare providers advocate for post-surgical protocols that include the use of mobile aids or exercises to promote circulation.
For individuals at higher risk of developing deep vein thrombosis (DVT) or PE, the use of compression stockings can be beneficial. These stockings exert gentle pressure on the legs, improving venous return and reducing the risk of clot formation. Additionally, maintaining a healthy weight is paramount, as obesity is a considerable risk factor for DVT and PE. A balanced diet and regular exercise can help achieve and sustain optimal body weight.
Smoking cessation is another significant step towards decreasing the risk of PE. Smoking adversely affects blood vessels and circulation, increasing the propensity for clot formation. Those who smoke should seek medical advice and resources to quit successfully. Adhering to all post-surgical care instructions given by healthcare providers is crucial. This often includes taking prescribed anticoagulant medications and attending follow-up appointments.
Regular medical check-ups and screenings are vital for those with a high risk of DVT or PE. Consistent monitoring can help catch early signs of potential issues, allowing for timely intervention. By incorporating these practical measures and making informed lifestyle choices, individuals can substantially lower their risk of pulmonary embolism, thereby enhancing their overall health and well-being.
Conclusion
In summary, pulmonary embolism (PE) is a serious medical condition that warrants attention due to its potentially life-threatening nature. Early detection is crucial, as it significantly increases the chances of successful treatment and recovery. Recognizing the common symptoms, such as shortness of breath, chest pain, and sudden onset of cough, can lead to quicker intervention and better outcomes.
Prevention remains a key aspect in managing the risk of pulmonary embolism. Measures such as maintaining an active lifestyle, staying hydrated, and following medical advice for managing underlying conditions like deep vein thrombosis (DVT) can be highly effective. Being aware of the risk factors, such as prolonged immobility, recent surgery, or a history of blood clots, is also essential for taking proactive steps to mitigate the risk of PE.
It is vital for individuals to take charge of their health by consulting healthcare professionals if they suspect any risk factors or exhibit symptoms of pulmonary embolism. Medical experts can provide personalized advice and appropriate interventions to reduce the likelihood of developing this condition.
We encourage readers to share this post to raise awareness about pulmonary embolism and its implications. By spreading knowledge, we can collectively contribute to early detection and prevention efforts, potentially saving lives. For more health-related information and updates, consider subscribing to our blog. Together, we can foster a well-informed community better equipped to tackle health challenges.
